Building on recent developments in biotechnology, biotech startup Frontier Bio has introduced a method to produce living human blood vessels in the lab. This innovation can potentially reshape the landscape of animal testing for vascular medical devices. With the Mayo Clinic, Frontier Bio successfully tested a device in a lab-made blood vessel that can redirect blood flow. Using 3D printing, the company can replicate complex vascular structures, mimicking natural and disease-related conditions. While Frontier Bio’s fusion of biology and technology hints at a distant future with reduced organ transplant needs, it has immediate potential in developing tools for blood clot removal.
Until now, animal studies have been a critical yet controversial step in evaluating the safety and performance of vascular medical devices. For instance, balloon angioplasty devices, designed to widen blocked or narrowed blood vessels, are typically tested in animals to ensure they can safely and effectively open up vessels without causing unnecessary injury. Similarly, vascular grafts, artificial vessels meant to bypass blockages, are studied in animals to see how well they integrate with natural vessels and if they resist clotting. Frontier Bio’s new approach promises a shift from this paradigm, aiming to reduce or eliminate the reliance on animal models to evaluate these devices.
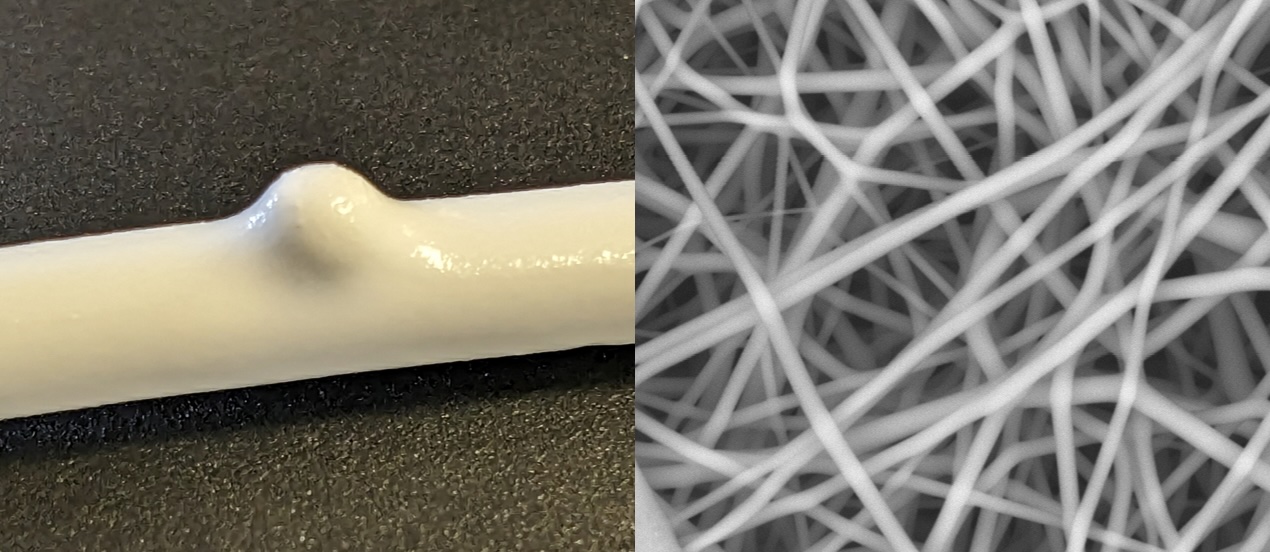
Frontier Bio’s new technique uses tissue engineering to grow these blood vessels in the lab. They do this by placing special cells onto a material that eventually breaks down on its own. Using conditions similar to how our body works and employing 3D printing technology, they can make these blood vessels in various shapes, including those that look like natural blood vessels or even ones with certain diseases.
In collaboration with Mayo Clinic, Frontier Bio has already demonstrated a real-world application of its innovation. As proof-of-concept, the startup created a tissue-engineered blood vessel with an aneurysm and deployed a vascular flow diverter device into it. This device, often used in medicine, directs flow away from an aneurysm, minimizing the risk of rupture. When tested with this device, the lab-grown vessel showed results parallel to those from traditional animal studies conducted on rabbits.
But when can we expect a complete transition from animal testing to these lab-grown vessels? Dr. Sam Pashneh-Tala, Frontier Bio’s new head of Vascular Tissue Engineering, weighs in: “Complete transition will take several years, probably over a decade. It will happen gradually, with some devices more easily transitioning than others.”

Sam Pashneh-Tala as the new Head of Vascular Tissue Engineering at Frontier Bio. Image courtesy of Pashneh-Tala.
Pashneh-Tala told 3DPrint.com that “momentum is growing. With the recent FDA Modernization Act 2.0, the regulations for animal alternatives in developing medical devices and drugs are becoming less of a barrier. The FDA’s emerging medical device development tool (MDDT) program offers a route for assessing new testing platforms. If their performance is acceptable, these can be used by device developers instead of animal models. Frontier Bio engages with this program to develop our tissue-engineered blood vessels (TEBVs).”
However, challenges remain. For one, proving the equivalent performance of these TEBVs compared to established animal models is a significant hurdle. “It will take time to build up this data,” Pashneh-Tala points out.
One of the major advantages of Frontier Bio’s approach, beyond the ethical implications, is cost. As Pashneh-Tala notes, “Certainly compared to large animal models, TEBVs have the potential to be cheaper and more reliable.”
The tissue engineering expert indicated they are very interested in employing its TEBV in developing thrombectomy devices, particularly in assessing acute vascular injury. Thrombectomy devices are inserted into blood vessels and used to remove blood clots. When being developed, these endovascular devices must be tested to see if they cause injury to the blood vessel wall when inserted, deployed, and removed. This acute vascular injury testing is usually done in pigs and is expensive and wasteful, with a single test costing between $10,000 and $20,000. Instead, TEBVs could provide the required data on vascular injury at a lower cost and without the need for animal sacrifice.
“The TEBVs we are developing as device testing platforms are designed to mimic real living vessels to the extent required for the specific application. Frontier Bio is also developing TEBVs as vascular grafts for implantation into patients to treat injury or disease. These will have the longevity and resilience of natural blood vessels,” points out Pashneh-Tala.
Additionally, the company harnesses 3D printing in novel ways to mimic complex vascular structures. “We produce our polymer scaffolds using electrospinning,” he shares. In simpler terms, they use 3D printing to design special molds that help shape these vessels, which allows them to recreate intricate blood vessel designs, even specific patient aneurysms, if required.
These molds guide the formation of incredibly fine fibers woven together to make a mesh-like scaffold. Once formed, this scaffold is filled with cells, which are then nurtured in lab environments designed to mimic human conditions, allowing them to grow into blood vessels. Moreover, they also craft special bioreactor chambers with 3D printing to grow the TEBVs in the lab. These are produced using SLA 3D printing from an autoclavable and biocompatible material, allowing the researchers to sterilize and use the parts in the lab effectively, explains Pashneh-Tala.
“3D printing enables us to design bioreactor chambers of varied shapes to fit any vessel geometry. These could even accommodate patient-specific vessel designs if needed. In the future, we are also interested in using 3D bioprinting techniques to generate TEBVs. Bioprinting allows us to deposit cells or aggregates of cells in a controlled manner, building up a 3D structure. This offers the potential for a wider range of vessel designs.”
Looking ahead, the company is setting its sights beyond just blood vessels. “Both neural and lung tissues may require more different cell types (more than three) than in blood vessels (2-3),” Pashneh-Tala notes, indicating the challenges and techniques differ when creating these tissues.
He elaborates on the unique challenges of tissue engineering, stating, “Vascularisation is a major challenge. Cells in tissues need proximity to blood vessels for nutrition. Tissue-engineered blood vessels side-step this problem, as they are the blood vessels. In other tissues, the network of blood vessels needed to support their cells must be engineered somehow. It could be produced directly as part of manufacturing or encouraged to grow spontaneously. One of the unique advantages of tissue engineering compared to other engineering disciplines is that our principal materials (cells) are not inert; they are both reactive and proliferative. With the correct stimulation, they can be encouraged to behave in certain ways and manufacture materials, such as collagen, or complex structures, such as microvascular networks, on their own. Finding the correct stimulation is the challenge.”
Pashneh-Tala remains optimistic about the broader implications for organ and tissue transplants. He believes It is likely that engineered tissues will make major impacts in the in vitro space in the next few years. This includes applications such as its TEBVs for testing medical devices and organ-on-a-chip technologies for drug development. The expert says that engineered tissues in the clinic have proven a formidable challenge, with only a handful of solutions reaching human trials over the past 30 years. “The outlook remains positive, and I expect these technologies to become more prevalent this decade.”
This breakthrough by Frontier Bio is a testament to the company’s commitment to leading-edge technology and ethics in the medical field. The future looks bright with the National Science Foundation (NSF) support and the recent incorporation of experts like Pashneh-Tala. As renowned geneticist with affiliations at Harvard University and MIT and advisor to Frontier Bio, George Church, puts it, “Frontier Bio is paving the way for a future where organ donors are no longer needed, and animal testing is a thing of the past.” Church’s expertise underscores the significance of Frontier Bio’s achievements in genetics and biotechnology.
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
Print Services
Upload your 3D Models and get them printed quickly and efficiently.
You May Also Like
3D Printing News Briefs, June 11, 2025: Sustainability, Automotive Tooling, & More
We’re starting with sustainability news in today’s 3D Printing News Briefs, as EOS has strengthened its commitment on climate responsibility, and Zestep is making 3D printing filament out of eyewear...
3D Printing 50 Polymer Stand-In Parts for Tokamaks at the PPPL & Elytt Energy
Of all the world’s things, a tokamak is one of the hardest, most complex, expensive and exacting ones to make. These fusion energy devices make plasma, and use magnets to...
3D Printing News Briefs, May 17, 2025: Color-Changing Materials, Humanoid Robot, & More
We’re covering research innovations in today’s 3D Printing News Briefs! First, Penn Engineering developed 3D printed materials that change color under stress, and UC Berkeley researchers created an open source,...
Firehawk Aerospace Partners with JuggerBot 3D, Gets $1.25M from AFWERX for 3D Printed Propellants
Texas-based Firehawk Aerospace, an advanced energetic materials firm that works with aerospace and defense applications, announced a strategic partnership with JuggerBot 3D, an Ohio-based large-format 3D printer manufacturer. Together, the...