Is Australia the land of bioprinting wonders? As news of the country’s efforts in bioprinting continues to emerge, it becomes clear that researchers are pushing the boundaries of medical science. Australia’s biotech industry has thrived for years as pioneering scientists take their discoveries to new heights.
Shortly after the University of New South Wales Sydney revealed a groundbreaking flexible robot that can bioprint inside the body, new exciting breakthroughs have been reported. Scientists at both the University of Sydney and the University of Technology Sydney (UTS) are laying the groundwork for the future of medical science by pioneering research and development in the field of artificial bioprinting, which has the potential to revolutionize organ transplantation in the next decades.
Mimicking organs
In a pivotal breakthrough, scientists from the University of Sydney bioprinted mini lungs in a dish to test medicines and potentially replace animal testing. Led by Wojciech Chrzanowski, a nanomedical researcher and academic at the Sydney Pharmacy School, and Huyen Phan, a postdoctoral research fellow at Westmead Institute for Medical Research, the investigation on lab-made lungs, known as organoids or mini-organs, serves as a testing ground for biomedical research.
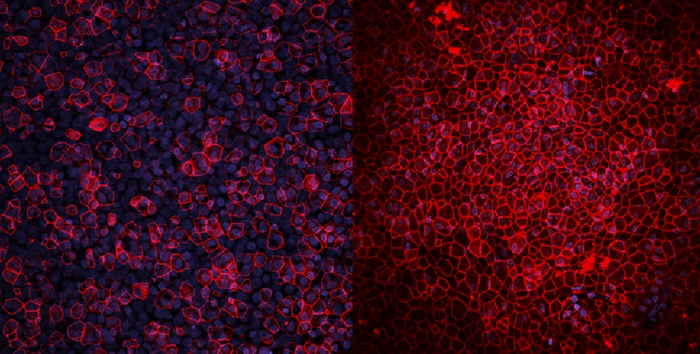
Model lung organoid under the microscope, diseased (left), healthy (right). Image courtesy of Phan et al.
Commenting on the study, which was published in the journal Biomaterials Research, Chrzanowski said: “We decided to build two different lung models, one which mimics phase one clinical trials; a healthy lung to study the safety of new drugs. The other one mimics phase two trials, a diseased lung that, in our case, mirrors chronic obstructive pulmonary disease, enabling us to study the therapeutic effectiveness or superiority of the drugs.”
Professor Chrzanowski explained that the models described in the paper, which are more accurate than traditional models, are unique in their ability to emulate the environmental conditions of a human lung. To mimic lung models, the team takes cells directly from patients and then builds them in layers as they exist inside the body.
Traditionally, the entire process of developing and obtaining regulatory approval for a new drug can take anywhere from 10 to 15 years or more, and it can cost hundreds of millions or even billions of dollars. However, Chrzanowski suggests that when using organoid models, this timeline shrinks substantially.
Development of these lung models brings Australia to the forefront of mini organ research, said Chrzanowski, who has been calling for establishing a national center for medical research alternatives to animal methods. In a bold move, Australia became one of the first countries to ban cosmetic testing on animals. Already in 1997, the government introduced a voluntary code of practice for the cosmetics industry that encouraged companies to use alternative testing methods to replace animal testing. Then, in 2017, a law was passed to ban the use of data from animal testing for cosmetics and the sale of cosmetics that had been tested on animals.
Chrzanowski’s mini-lungs are the latest in a decades-long career designing and developing nanomaterials for medical applications. In addition, the expert has researched bioprinting as part of his broader work in the field of biomaterials science and engineering and explored various aspects of bioprinting, including developing new biomaterials and optimizing printing techniques to improve the accuracy and functionality of printed structures. Overall, his work in bioprinting and related fields has contributed significantly to our understanding of how nanotechnology can be used to advance medical research and treatments.
Bioprinted patches
Another major triumph for Australian academics is a recent UTS breakthrough in demonstrating that bio-engineered heart tissues can safely and effectively help patients recover from the damage caused by an extensive heart attack.
A new bioprinting study published in the journal Bioprinting showcases a significant step forward in developing a new technology that creates personalized bioinks made of a patient’s own stem cells, which are then used to 3D print cardiac tissues to repair areas of dead tissue caused by cardiac failure.
Cardiology research pioneer Carmine Gentile led a preclinical study – using mice as animal models – to help better understand how bioengineered heart tissues work in the body after their transplantation.
“Our study demonstrated that bio-engineered patches were the best and most robust treatment of heart failure – patches generated with other approaches either did not induce any improvement or the improvement was inconsistent,” indicates Gentile, who heads the Cardiovascular Regeneration Group at UTS. “Our bio-engineered patches promise to be safer, more consistent, and cost-effective for the patient.”
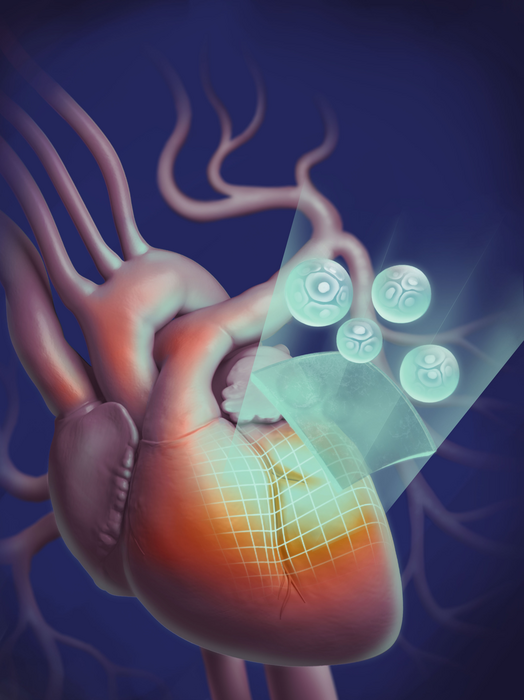
Bioniks used to 3D print cardiac tissues to repair areas of dead tissue caused by heart attacks. Graphics courtesy of Leo Herson.
These 3D printed human tissue constructs use a novel hybrid bioprinting approach that combines living cells and biomaterials to create functional tissues. Printed with a BIO X pneumatically driven extrusion 3D bioprinter by pioneering firm Cellink (a subsidiary of BICO) and a bioink made of cardiac cells mixed with AlgGel (a hybrid material composed of alginate and gelatin), the patches were surgically transplanted to the epicardial surface of mouse hearts.
The study titled “3D bioprinted alginate-gelatin hydrogel patches containing cardiac spheroids recover heart function in a mouse model of myocardial infarction” concludes that 3D bioprinted hydrogel patches with unaltered cardiac spheroids can improve cardiac function when transplanted onto the outermost layer of a mouse’s heart.
“Because this technology will enable patients to use their own stem cells to create the heart ‘patches,’ not only can they potentially dramatically reduce the trauma and cost of a heart transplant, but also avoid hurdles such as a body rejecting donor tissues,” illustrated Gentile.
Further testing for the long-term effects of this technology is already underway before starting clinical trials.
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
You May Also Like
Profiling a Construction 3D Printing Pioneer: US Army Corps of Engineers’ Megan Kreiger
The world of construction 3D printing is still so new that the true experts can probably be counted on two hands. Among them is Megan Kreiger, Portfolio Manager of Additive...
US Army Corps of Engineers Taps Lincoln Electric & Eaton for Largest 3D Printed US Civil Works Part
The Soo Locks sit on the US-Canadian border, enabling maritime travel between Lake Superior and Lake Huron, from which ships can reach the rest of the Great Lakes. Crafts carrying...
Construction 3D Printing CEO Reflects on Being Female in Construction
Natalie Wadley, CEO of ChangeMaker3D, could hear the words of her daughter sitting next to her resounding in her head. “Mum, MUM, you’ve won!” Wadley had just won the prestigious...
1Print to Commercialize 3D Printed Coastal Resilience Solutions
1Print, a company that specializes in deploying additive construction (AC) for infrastructure projects, has entered an agreement with the University of Miami (UM) to accelerate commercialization of the SEAHIVE shoreline...