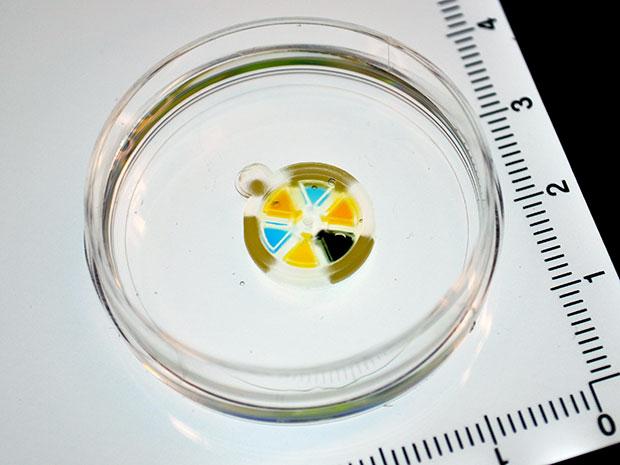
 A Geneva drive is a two-geared mechanism which turns a continuous rotation into an intermittent rotary motion, thus producing very precise ticks forward. It was developed by Swiss watchmakers, and is still used today in movie projectors, the machines that banks use to count money, and even this cool 3D printed Stargate mechanism. But now, bioengineers at Columbia University have created a 15-millimeter Geneva drive, using squishy hydrogel, in order to make a biocompatible micromachine that can be used to deliver doses of drugs on command once it’s been implanted inside your body. Think about it – you wouldn’t have to keep watching the clock to determine if it’s time for your next dose yet! The device was created in the Sia Lab, where the principal investigator, Columbia University professor of biomedical engineering Samuel Sia, spends his days working with microfluidics.
A Geneva drive is a two-geared mechanism which turns a continuous rotation into an intermittent rotary motion, thus producing very precise ticks forward. It was developed by Swiss watchmakers, and is still used today in movie projectors, the machines that banks use to count money, and even this cool 3D printed Stargate mechanism. But now, bioengineers at Columbia University have created a 15-millimeter Geneva drive, using squishy hydrogel, in order to make a biocompatible micromachine that can be used to deliver doses of drugs on command once it’s been implanted inside your body. Think about it – you wouldn’t have to keep watching the clock to determine if it’s time for your next dose yet! The device was created in the Sia Lab, where the principal investigator, Columbia University professor of biomedical engineering Samuel Sia, spends his days working with microfluidics.
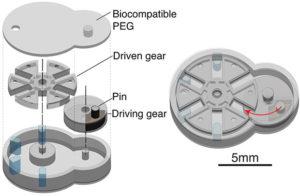
The Geneva drive micromachine doesn’t utilize batteries or wires: these drives traditionally work by adding a driven wheel to the gear, which has slots, and advances a single step of 90° each time the wheel rotates. Sia’s micromachine platform, formally titled “implantable microelectromechanical systems (iMEMS),” can be used to deliver a dose of medicine on command, and is controlled from outside the body. This way, doctors who prescribe the medicine are able to see how their patient is faring, and then modify any medicinal therapy if necessary. Sia has already tested the iMEMS in lab mice with osteosarcoma (bone cancer), and the positive results were published yesterday in the Science Robotics journal. The abstract for the experiment explains that by “exploiting the unique mechanical properties of hydrogels, we developed a locking mechanism for precise actuation and movement of freely moving parts.”
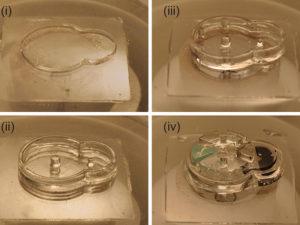
The researchers constructed their Geneva device layer by layer, in a process that took about 30 minutes.
Sia explained that the hardest part was getting the material just right. While soft, flexible materials are compatible with what’s inside your body, “if your material is collapsing like jello, it’s hard to make robots out of it. It has to be stiff enough to work like a tiny implantable machine.” The team actually had to invent a different type of 3D printing in order to create the small Geneva drive, and created a fabricator that is able to produce rubbery, solid shapes by layering the squishy hydrogel.
Sia says that in the future, assembly of the pieces can be automated, but right now, human hands are necessary to put the pieces together. Even without automation, the entire printing and assembly process for one small, implantable Geneva drive takes less than half an hour.
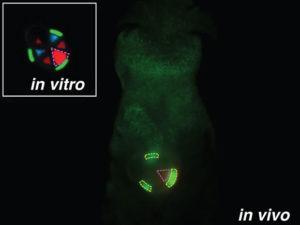
The video below shows how the iMEMS works. It will click forward, on command, when an external magnet moves a rubbery gear that has been embedded with iron nanoparticles. Each time the device clicks, one of six total chambers will line up directly with a hole, and a dose of medicine comes out of the hole. In actual clinical use, a physician would be able to apply the magnet only when a dose is required, but for the purpose of demonstrating how the device works in the video, a silver magnet keeps it running continuously.
While it’s unlikely that someone’s implanted micromachine will be triggered by someone walking past them with a magnet, Sia admits that “there are some cases where it’s not ideal.” His lab is working to develop different ways to drive the device without magnets, including an ultrasound technique.
Some of the lab mice with bone cancer were implanted with iMEMS that contained the chemo drug doxorubicin, while others were treated with typical chemotherapy. When Sia’s team compared the traditional treatment with the effects of their device’s periodic and localized drug delivery over ten days, they were thrilled to see that with the latter treatment, the tumors in the mice grew more slowly, more tumor cells died, and fewer cells throughout the body were damaged. If this device is able to be used in the real world, the clinical benefits would be great – hormone release could be regulated, and oncologists would be able to deliver more concentrated doses of chemotherapy drugs, increasing the quality of life in their patients. But Sia says this is simply a proof of concept.
“We have to do the cost-benefit analysis to see if this is really a commercializable device.”
This doesn’t mean that he’s done yet, though. His team’s groundbreaking fabrication platform is able to create many small, soft devices, and he is “confident that we’ll find something useful.” Discuss in the 3D Printed Hydrogel forum at 3DPB.com.
[Source: IEEE Spectrum / Images: Sau Yin Chin]
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
You May Also Like
Further Understanding of 3D Printing Design at ADDITIV Design World
ADDITIV is back once again! This time, the virtual platform for additive manufacturing will be holding the first-ever edition of ADDITIV Design World on May 23rd from 9:00 AM –...
3D Printer Maker EVO-tech Reborn as NEVO3D — Once More With Feeling
EVO-tech was a 3D printing service and original equipment manufacturer established in 2013 and based in Schörfling am Attersee, Austria. The company produced high-quality material extrusion systems featuring linear bearings,...
3D Systems Brings 3D Printed PEEK Cranial Implant to the U.S. with FDA Clearance
For more than 10 years, 3D Systems (NYSE:DDD) has worked hand-in-hand with surgeons to plan over 150,000 patient-specific cases, and develop more than two million instruments and implants from its...
CDFAM Returns to Berlin for Second Annual Symposium
The second CDFAM Computational Design Symposium is scheduled for May 7-8, 2024, in Berlin, and will convene leading experts in computational design across all scales. Building upon the first event...