During the recent 3D Systems’ 2014 Investor & Analyst Day, one of the key issues addressed was the new frontiers in medical technology. At 3D Systems, healthcare appears to be the fastest growing market. The  management team stated its plans to build up its leadership in this field. The company plans to invest and expand its virtual surgical planning (VSP®) capabilities, broaden its range of implants and surgical tool manufacturing and develop new personalized medical devices, such as the recently introduced bespoke scoliosis brace.
management team stated its plans to build up its leadership in this field. The company plans to invest and expand its virtual surgical planning (VSP®) capabilities, broaden its range of implants and surgical tool manufacturing and develop new personalized medical devices, such as the recently introduced bespoke scoliosis brace.
In April, 3D Systems announced the acquisition of Medical Modeling, a leading provider of personalized surgical treatments and patient specific medical devices, including virtual surgical planning (VSP®). The VSP is a service-based approach to personalized surgery that combines expertise in medical imaging, surgical simulation and additive manufacturing. It allows for planning maxillofacial surgical procedures in a virtual environment and transferring that plan to the patient using innovative models, templates and surgical guides manufactured with 3D printers. Recently, it was used by Dr. Oren Tepper, Assistant Professor of Surgery at New York’s Montefiore Medical Center and a pioneer in virtual surgical planning. He performed surgery on a 3-week-old girl named Jayla Vargas who had difficulty breathing due to her tiny jaw. Traditionally, in such cases, she would have had to wait 6 years until she was large enough for the operation. However, with the help of VSP technology, Dr. Tepper successfully fixed Jayla’s jaw.
At the Investor & Analyst Day, Dr. Oren Tepper was the guest speaker and he discussed the current uses and future applications of 3D printing in plastic surgery. Dr. Oren Tepper explained how technology is important in plastic surgery as creativity and innovation are involved in building, restoring and renovating the human body. Therefore, practitioners embrace this technology. Over the last several years, training and skills have been the key points in technical innovation related to plastic surgery. Advanced techniques have been used and cutting edge technology has been incorporated. For the moment, all of these advancements are focused on the operating room itself. Nonetheless, this technology is bringing greater planning and precision to operating rooms, enabling surgeons to perform successful operations that were previously impossible.
At the moment, 3D Systems and Medical Modeling has had a tremendous impact on bone reconstruction, but it is still a relatively small impact in the field. The untapped potential, especially in soft tissue reconstruction, is enormous.
“This technology eliminates surprises, minimizes complications and improves the precision of surgery.”
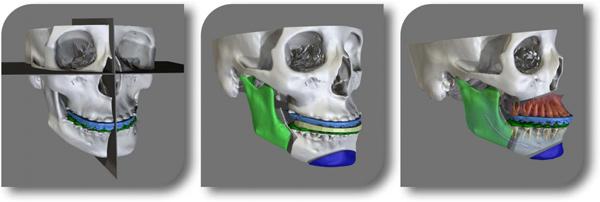
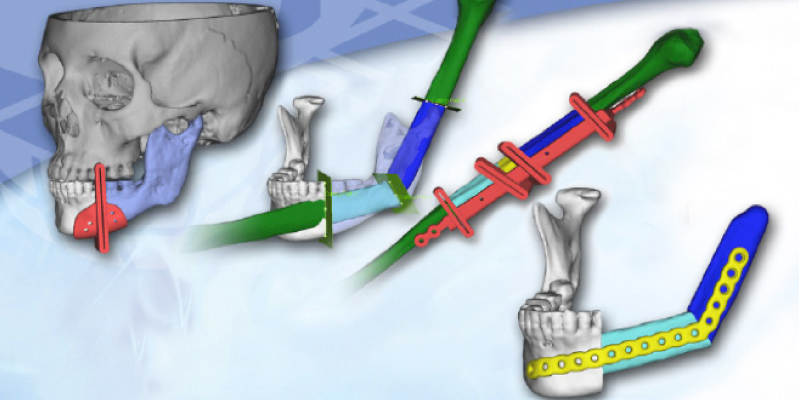
According to the doctor, the first real advancement was the CT scanner, which allowed plastic surgeons to look at bodies via the CT scans. Next, the skull was 3D printed so it could be used as a reference. The process started building stereolithographic models of the skulls so it was possible to study them in any direction and to practice surgery. That was the first generation, just printing the existing anatomy of the patient. Now, it is possible to plan a surgery on a computer for surgical simulation. Therefore, surgeons can move the bone structures where they want them to be and they can develop on the computer and 3D print guides and jigs which they sterilize and bring to the operating room.
possible to plan a surgery on a computer for surgical simulation. Therefore, surgeons can move the bone structures where they want them to be and they can develop on the computer and 3D print guides and jigs which they sterilize and bring to the operating room.
The first study about virtual surgical planning and printing was published 5 years ago. Regarding facial fractures, Dr. Tepper used an example at the conference of a lower jaw fractured in multiple pieces, on a young woman named Jayla. Due to limited exposure of the surgeon and the lack of reference points, it was difficult to put the jaw back together. The phases to follow during the process of reconstruction are:
- Phase 1. Virtual planning: Reduce fracture and establish occlusion on the computer.
- Phase 2. Modeling: Create jigs and guides that can be taken to the operating room.
- Phase 3. Surgering. Place the 3D printed jigs on the patient in the operating room and use them to put the facial fractures together.
- Phase 4. Analysis: Achieve what doctors have automatically set out to do surgically.
Regarding Jayla’s operation, Dr. Tepper emphasized that the procedure used was safer and cheaper than the traditional practice, a tracheostomy, which is a surgically created opening in the windpipe to allow proper breathing. However, virtual surgical planning is only used on a small percentage of operations today. When asked about the challenges he faced and the solutions that he came up with, Dr. Tepper highlighted four reasons why 3D printing was so useful to him in the operating room:
- The device size. He wasn’t sure if the device was small enough that it would fit under the lower jaw but this technology solved that problem.
- The underdevelopment of the patient’s bone. Jayla’s bone was so under developed that he needed to place the device exactly at the same parallel vector. Again, thanks to this computer technology he could perfectly do just that.
- The critical structures. The lower jaw is not just simply made of bone. Thanks to the computer, it was possible to identify the different structures and stay away from those critical structures.
- The bone width. This technology allowed him to predict the size of the bone so he knew exactly where to place the device.
Dr. Tepper believes in the technology’s future growth potential as it will make the existing infrastructure better and faster and it will represent a tremendous opportunity in expanding markets. At the moment, there is no communication between plastic surgeons and 3D printing companies. On the contrary, it is an opportunity for real time communication so that companies like 3D Systems could have a role in the operating room. Dr. Tepper affirmed that surgeons will one day look back on non-VSP procedures as crude and primitive.
How long will it be before this type of technology is commonplace within the operating room? Let’s hear your thoughts in the 3D printing and surgery forum thread on 3DPB.com.
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
You May Also Like
Precision at the Microscale: UK Researchers Advance Medical Devices with BMF’s 3D Printing Tech
University of Nottingham researchers are using Boston Micro Fabrication‘s (BMF) 3D printing technology to develop medical devices that improve compatibility with human tissue. Funded by a UK grant, this project...
3D Printing Webinar and Event Roundup: April 21, 2024
It’s another busy week of webinars and events, starting with Hannover Messe in Germany and continuing with Metalcasting Congress, Chinaplas, TechBlick’s Innovation Festival, and more. Stratasys continues its advanced training...
3D Printing Webinar and Event Roundup: March 17, 2024
It’s another busy week of webinars and events, including SALMED 2024 and AM Forum in Berlin. Stratasys continues its in-person training and is offering two webinars, ASTM is holding a...
3D Printed Micro Antenna is 15% Smaller and 6X Lighter
Horizon Microtechnologies has achieved success in creating a high-frequency D-Band horn antenna through micro 3D printing. However, this achievement did not rely solely on 3D printing; it involved a combination...